Spray, don’t delay! conversations around naloxone in practice
The Current State of the Opioid Crisis
17 Canadians die from opioid toxicity each day, 96% of which are accidental.1 During the rise of the COVID-19 pandemic from 2019 to 2020, opioid-related hospitalizations increased by 23% and opioid toxicity deaths increased by 89%.1 Fentanyl and its analogues continue to be the main drivers of opioid toxicity, constituting 82% of accidental opioid toxicity deaths last year.1 There is a clear need for more proactive intervention in order to curb the rising fatalities related to opioid use.
Updates to Canadian Guidelines on Naloxone Prescribing
Naloxone is an opioid antagonist with a strong affinity for opioid receptors. It is an effective but temporary antidote that displaces opioids at receptors to reverse opioid-induced respiratory depression and prevent opioid-related deaths.2 Naloxone is available as an injectable solution (0.4mg/dose) and as a nasal spray (NARCAN®, 4mg/dose).2 Naloxone is designated as Schedule II by NAPRA, although the schedule in individual provinces may differ (unscheduled in BC, AB, and SK). Each province also has its own publicly funded take-home naloxone (THN) program, with the aim of increasing accessibility and removing financial barriers associated with accessing naloxone, however, not all provinces currently involve pharmacies in these programs.3 The formulation of naloxone covered provincially also differs; although intra-nasal naloxone is easier to use and is associated with less risks (e.g., no needlestick injuries), many provinces have not yet adopted its use for their THN programs. Both forms of naloxone are fully covered for eligible patients under the Non-insured Health Benefits (NIHB) Program and Veterans Affairs Canada.
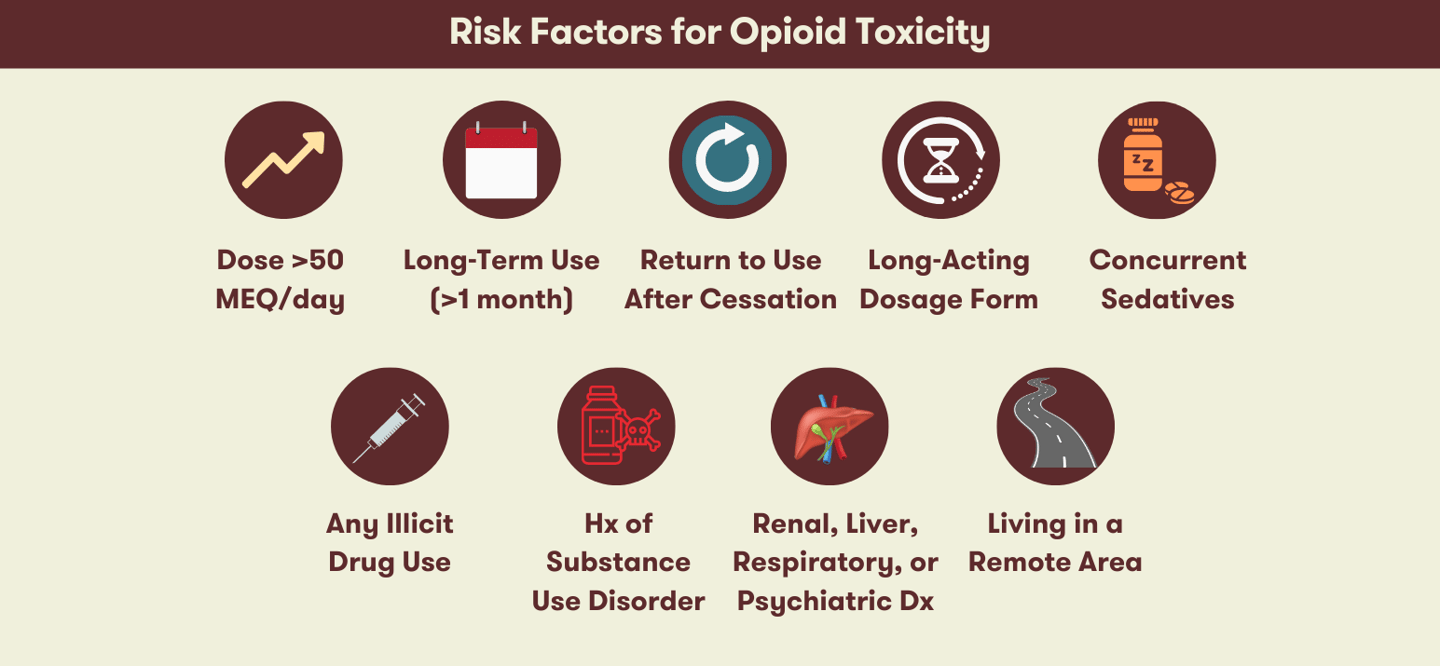
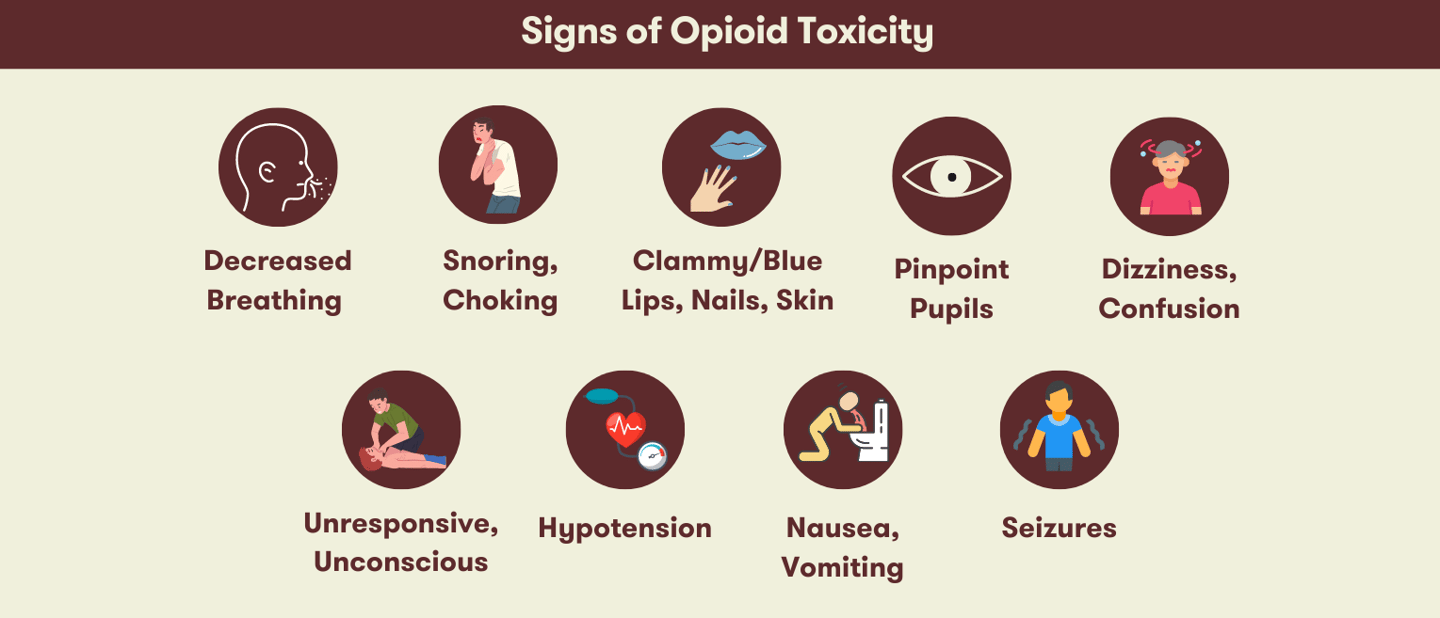
In Ontario, up to one third of opioid-related deaths involve prescription opioids.3 When it comes to offering naloxone to patients, the newest Canadian pharmacist guidelines on naloxone prescribing recommend counselling and dispensing naloxone to all patients receiving an opioid.3 This is a change from previous recommendations to select patients based on certain risk factors (e.g., history of overdose, concomitant use of other sedatives, presence of mental health disorders, suspected illicit use of opioids, etc.). Although there are certain individuals who are more at risk of opioid toxicity than others, it is difficult to determine which patients possess certain risk factors, as patients may be unlikely to disclose this information due to the stigma associated with substance use disorders or due to the legalities of using drugs from illicit sources.3 The use of multiple pharmacies also makes it difficult to identify if the patient is taking other medications that can increase their risk, such as sedatives like benzodiazepines or other CNS depressants.3 It is also important to highlight that the risk of opioid toxicity can affect other family members in the household such as young children or elders who may accidentally ingest the patient’s medication.3 Thus, it is best to offer naloxone to everyone with an opioid prescription as a safety net to proactively reduce the risk of opioid-related deaths among patients and those around them.
What Pharmacists Can Do
Most individuals recognize the dangers of opioids, however they rarely internalize that they are at risk of opioid toxicity themselves and often experience a false sense of security.3 “Overdose” is usually perceived as a self-inflicted phenomenon that happens as a result of taking “too much” illicit opioids; as a result, it is rarely recognized as an adverse effect of opioids that might affect ourselves or our loved ones. Patient refusal is often a leading barrier to dispensing naloxone, even in scenarios where there is no cost to the patient. There is a marked need for pharmacy awareness campaigns to address the stigma around opioid use and naloxone, and for health care professionals to close this gap through comprehensive patient education.
As the most accessible health care professionals, pharmacists are well-positioned to identify patients to initiate conversations around naloxone. By counselling each and every patient with an opioid prescription and using neutral language that reduces stigma, we can normalize these conversations and increase the uptake of naloxone to effectively prevent opioid-related deaths.3 Language can make a big difference during patient interactions around naloxone. For example, you may have noticed that throughout this article we prefer the terminology opioid “toxicity” instead of “overdose”. “Toxicity” is a more accurate descriptor that puts the blame back on the nature of the drug instead of the acts of the individual, as insinuated by “overdose”.6 Alternative phrases include “accidental/unintentional opioid poisoning”, or when speaking to other healthcare professionals, “opioid-induced respiratory depression”. Framing “opioid overdose” in a way that shifts perceived blame away from individuals can help improve buy-in from patients who may feel stigmatized from discussions around naloxone.6
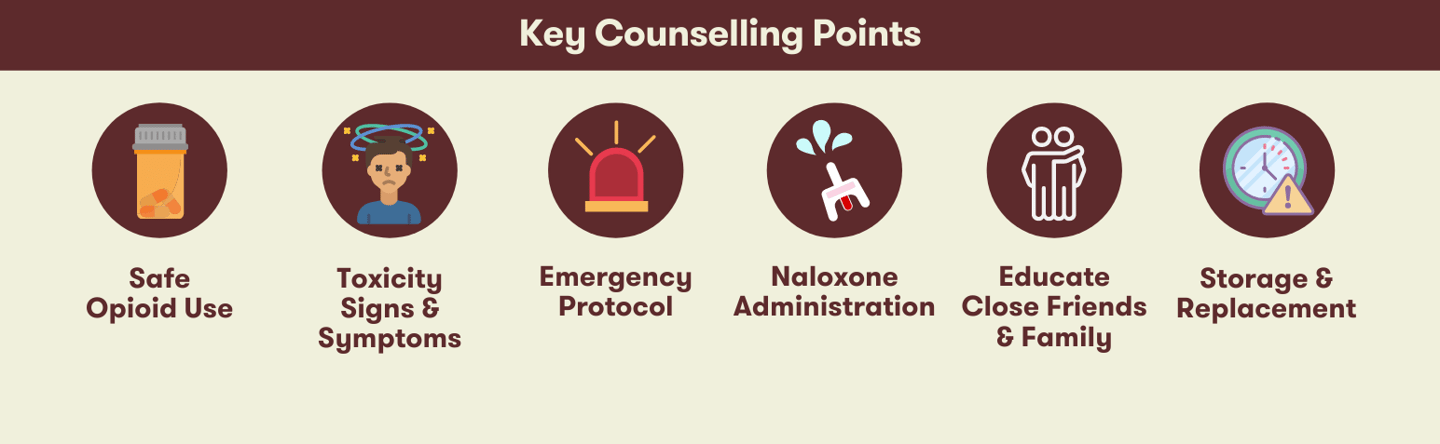
Educating patients on prevention strategies such as safe opioid use and storing them in a lock box is another critical component of the pharmacist’s role in counselling patients with opioid prescriptions.3 It is also important to train patients to recognize and respond to opioid toxicity, including proper administration of naloxone.3 For ongoing monitoring, pharmacists should follow-up with patients who have received naloxone annually to check on the expiry date and refill their naloxone if necessary, refresh their knowledge on naloxone, and ask about any changes in opioid prescriptions or other risk factors.3
It is also important for all healthcare workers to assess stigma within our own practice and environment. Evaluating preconceptions and implicit biases within our pharmacy teams is essential to ensure consistency in establishing a safe space to discuss opioid use and naloxone. Continued advocacy and awareness campaigns are needed at each level to battle stigma and ensure equitable access to naloxone. Pharmacy distribution is proven to be successful in improving uptake of naloxone. Pharmacies are key players and additional resources and support for widespread engagement of pharmacy in naloxone programs would only benefit our patients and communities.
Wholehealth has developed a program addressing opioid toxicity, the benefits of naloxone, and the role of pharmacy teams in reducing stigma and preventing opioid-related deaths. Be sure to follow us on social media for up-to-date patient awareness materials! If you would like more information or resources from our campaign such as our webinar, please e-mail [email protected].
References
- Special Advisory Committee on the Epidemic of Opioid Overdoses. Opioid- and stimulant-related harms in Canada. Government of Canada. Updated June 23, 2021. Accessed Jul 13, 2021. https://health-infobase.canada.ca/substance-related-harms/opioids-stimulants/
- Naloxone. In: Lexi-Drugs. Lexi-Comp, Inc. Updated July 13, 2021. Accessed July 13, 2021. www.online.lexi.com
- Tsuyuki RT, Arora V, Barnes M, et al. Canadian national guidelines for naloxone prescribing by pharmacists. Can Pharm J. 2020;153(6):347-351. doi: 10.1177/1715163520949973
- Schiller EY, Goyal A, Mechanic OJ. Opioid overdose. In: StatPearls [Internet]. StatPearls Publishing LLC; 2021. Accessed July 13, 2021. https://www.ncbi.nlm.nih.gov/books/NBK470415/
- Coffin, P. Prevention of lethal opioid overdose in the community. In: Post T, ed. UptoDate. UpToDate; 2021. Accessed July 13, 2021. www.uptodate.com
- Xie E, Green S, Puri N, Sheikh H. Updating our language around substance use disorders. CMAJ. 2017 Dec 18;189(50):E1566. doi: 10.1503/cmaj.733490