Refresher on gout: the only curable arthritis
Gout is the most common inflammatory arthritis, yet it is frequently underdiagnosed, misdiagnosed and often mistreated.
Yet, according to rheumatologist Dr. Jean-Philip Deslauriers, once patients are on the right treatment, it’s the only arthritis where a cure can be achieved.
“With other arthritis conditions, the goal is remission. But with gout one can get rid of the underlying disease and attain a cure,” he said. Dr. Deslauriers is a clinical professor of medicine at the University of Sherbrooke and spokesperson for the Arthritis Society of Canada (ASC).
“Gout is easy to treat, and most cases can be managed by family doctors,” told the Medical Post in an interview. Gout is a painful arthritis caused by elevated levels of serum uric acid (UA), hyperuricaemia.
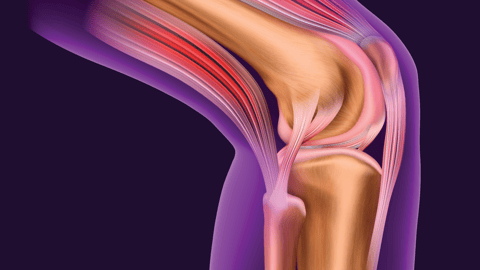
Prolonged hyperuricaemia (which is generally asymptomatic and can be present for years) leads to the deposition of monosodium urate crystals in synovial fluid and other body tissues. Eventually, neutrophils will venture into the joint to try to destroy the crystals (partly unsuccessfully) but end up triggering an episode of painful inflammation—a gout crisis in which patients present with inflamed, painful and swollen joints. Often, but not always, the affected joint is in the foot or ankle, especially the first metatarsophalangeal joint.
Crystals can also be deposited in other tissue and sometimes break through the skin creating yellowish-white nodules called tophi.
There are several reasons why gout can be missed. One is that symptoms are intermittent and it can take years for crystals to build up inside joints. A patient may present to an outpatient clinic or ER where acute symptoms are treated with colchicine, NSAIDs, cortisone infiltration or prednisone for their acute crisis, and then sent home and told to see their family physician for follow-up.
Crisis and oft missed opportunity
But a crisis, in the early stage of the disease, tends to last for only three or four days. By the time patients see an FP, they feel fine and may not mention it—if they even have access to an FP.
“Often there is only management for the crisis itself. If we don’t address the underlying cause which is too much uric acid in their blood, crises will happen again, more intensely and more frequently. And the disease will affect more joints. Over time this can lead to deformity and erosion, possible crystal formation in soft tissue called tophi,” Dr. Deslauriers said.
According to the 2018 recommendations for gout by the European League Against Rheumatism (EULAR), several features need to be taken into account for a diagnosis. These are: monoarticular involvement of a foot or ankle joint; previous acute episodes; rapid onset of severe pain and swelling; erythema; being male and associated cardiovascular diseases, plus hyperuricaemia.
For a definite diagnosis, crystals need to be seen in synovial fluid or tophus aspirates.
Both the EULAR and American College of Rheumatology (ACR) guidelines state that once gout is confirmed, treatment to lower UA levels can start even while the patient is in crisis
“This is a very important point because if not done when the patient is assessed during his acute crisis, it often isn’t done at all,’’ Dr. Deslauriers said.
But before prescribing drugs, review the patient's other medications, as some may be responsible for causing an increase in UA values, he noted. “One set of culprits are the diuretics thiazine and thiazine-like drugs which reduce the capacity of the kidney to excrete uric acid.”
“If it is appropriate, sometimes switching thiazine or thiazine-like to losartan or a calcium channel blocker can help their kidney better filter the UA and lower levels. If that works it prevents adding another medication to their regime,” he said.
There are several drugs designed to lower UA levels, the most common being allopurinol which helps the kidneys eliminate more uric acid.
Addressing the root causes
But, how do UA levels become elevated in the first place? It is simply an imbalance between the production and elimination of UA. Aside from suspect medications, there are several reason for this .For most people diet, weight and kidney function along with a genetic predisposition, are key.
Certain foods contain purine which are later metabolized to UA. According to the ACR, higher risk foods include red meat, organ meat, alcohol, shellfish, oily fish like sardines and mackerel, and foods containing corn syrup. The DASH diet and related healthy diets have been found to be mildly beneficial.
Being overweight or obese are associated with more gout crises, so a healthy weight is important too, said Dr. Deslauriers. Heavier people tend to have more muscular mass and are at greater risk because UA production is associated with the normal degradation of muscles.
People with kidney disease have increased risk for gout, but gout can, in turn, also be a sign of kidney disease in some patients.
Trusting the (lengthy) process
Lowering UA levels and removing crystals deposited in the joints can take time—often as long as it took for crystals to build-up. For a patient with earlier disease, this might mean being on allopurinol for a couple of years. If UA levels were elevated for a decade or more and there is substantial crystal deposition, treatment may need to continue for about as long, Dr. Deslauriers said.
Treatment needs to be titrated according to the UA serum values—and this should be monitored periodically so the dose of allopurinol can be adjusted.
According to ACR recommendations for the management of gout, “Urate-lowering therapy is recommended for patients with two or more gout flare-ups per year, tophaceous gout, or damage attributable to gout visible on radiography.” It adds that urate-lowering therapy can be started “during an acute flare-up instead of waiting until it resolves. Therapy started during a flare-up does not increase or prolong symptoms as long as anti-inflammatory treatments are provided.”
Adding anti-inflammatory treatments along with UA-lowering medication is vital in the first few months because there is an apparent paradox with treatment – it can trigger another gout crisis. When UA levels first start to be lowered, it attracts neutrophils to the joints where they cause short-term inflammation by attacking remaining crystals. Anti-inflammatory treatments such as NSAIDs can prevent this. Patients with erosion or tophis usually need to take these for a longer duration.
“Once you no longer have UA crystals in your joints you are cured,” Dr. Deslauriers said.