Ow, ow, ow! A refresher on plantar fasciitis
Plantar fasciitis: It can be a real pain for patients—and often lasts months, even years.
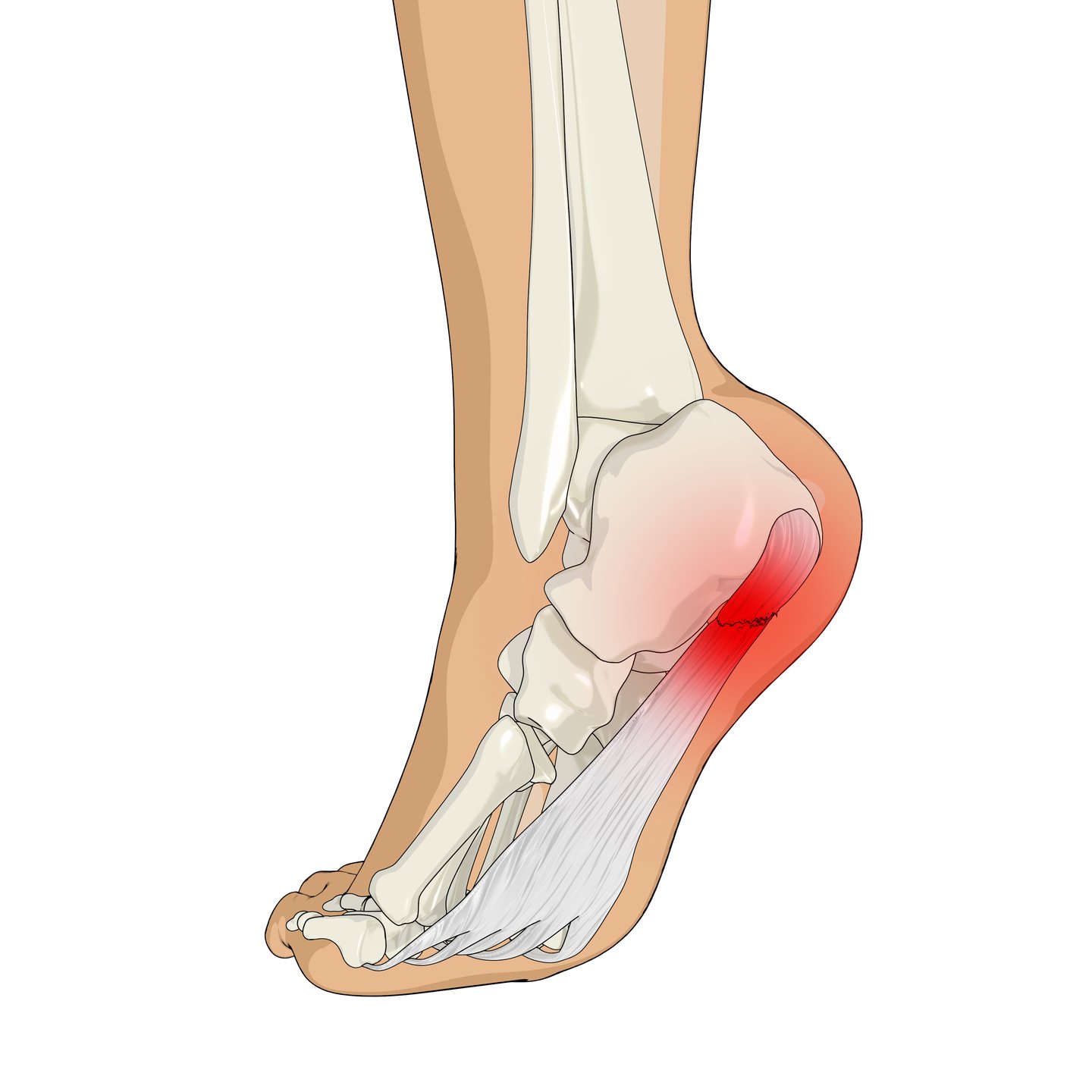
An inflammation of the plantar fascia, a thick band of tissue on the bottom of the foot, it’s the most common cause of heel pain and usually comes with significant arch pain as well.
Cases often multiply in the warmer weather, not just because patients become more active, but because going barefoot or wearing unsupportive footwear like flip-flops becomes more common. But at any time of year, simply being at home and going shoeless, as when working from home, can create the inflammation that leads to stabbing heel and arch pain.
“Here on the West Coast people start early in the year training for runs and marathons that can lead to heel pain and plantar fasciitis,” said doctor of Podiatric Medicine Jenny Ling, who is based at Metrotown Podiatry in Burnaby, B.C. “But it’s not just the weekend warriors who can be afflicted. It could be that patients are working from home, without supportive footwear, walking around in bare feet or socks all day long.”
Another contributing factors could a job or lifestyle that requires someone regularly being on their feet all day. A patient's weight can also come into play.
Plantar fasciitis occurs in about 10% of the general population, with 83% of these patients being active working adults between 25 and 65 years. About one-third of the time, it affects both feet. The condition can be stubborn, with some estimates stating it lasts three to six months. According to Plantar Fasciitis in StatPearls, 2024, by lead author Dr. Benjamin K. Buchanan, a sports medicine physician, about 70%-to-80% of patients with plantar fasciitis see symptom reduction only in nine to 12 months, with at least 5% to 10% requiring surgical plantar fascia release.
Common differential diagnosis
- Heel spurs often coexist with plantar fasciitis but aren’t usually the primary pain generator.
- Achilles tendinitis causes posterior heel pain, especially in active individuals.
- Posterior tibial tendinopathy or flatfoot collapse may explain medial arch pain, while cavus foot (high arches) can drive lateral arch discomfort.
- Neuropathic causes (like tarsal tunnel syndrome, when the tibial nerve is damaged) should be suspected when heel pain comes with burning or numbness.
- Heel bursitis causes low posterior heel pain, which worsens as the day goes on.
- Osteoarthritis usually affects more than the heel/arch and worsens with activity.
- Calcaneal (heel bone) stress fractures are more common with osteoporosis.
Plantar fasciitis is a clinical diagnosis, and imaging is usually unnecessary, according to Plantar Fasciitis. Best practice is to start with a good history: When did the pain begin? What activities or footwear aggravate it? Is there a history of overuse or biomechanical issues? A focused exam assessing gait, tenderness points, arch structure, Achilles flexibility and neurologic status will usually point you in the right direction.
Clinical exam
A key clinical indicator of plantar fasciitis are stabbing pain with the first steps in the morning that gradually improves. Pain typically lessens with initial movement or the start of physical activity but tends to worsen as activity continues throughout the day. Tenderness is often elicited by palpating the plantar medial calcaneal tubercle, where the plantar fascia inserts into the heel. Discomfort can also be reproduced with passive dorsiflexion of the foot and toes.
X-rays or ultrasound evaluation may be warranted if history or physical exam indicates other injuries or conditions or the patient fails to improve after a few months. X-rays and ultrasound evaluation may show calcifications in the soft tissues or heel spurs. MRI may come into play for refractory or complex cases.
Not just a local problem
Ling says that physicians need to know that plantar fasciitis is not just a localized issue.
“It can be more of a postural problem that manifests in plantar fasciitis,” said Ling, a Canadian Podiatric Medical Association board member. “You have to deal with the local inflammation at the heel, but you may not be fully successful if the root cause is postural. You have to look further up the kinetic chain, and it should be treated promptly before it seriously affects other joints and muscles.”
Tight calves, for example, could be connected to plantar fasciitis. “People don't have tight calves in isolation. Usually that also means that they have tight hamstrings and tight glutes, knee pain, or hip or low back pain, even the pelvic floor,” she said.
Jenga blocks
It’s kind of like Jenga blocks, she said: If one area is out of alignment then the body adjusts with different compensations, possibly by pushing another area to go out of alignment.
“Your body and your brain are constantly just trying to maintain a straight spine. This is what orthotic therapy, in conjunction with a strength and stretch program, addresses.”
Ling says when treating a patient with plantar fasciitis, her approach is multifactorial, starting with proper icing technique (See guidelines below). “Proper icing can be more helpful than prescribing systemic anti-inflammatories because it's really hitting it right where you need to,” she said.
A key consideration and point of discussion in Ling’s clinic is looking at patient shoes—what they are wearing in the house as well as for physical activities. Orthotics are not always necessary, but when they are prescribed, the shoes need to be right. “Even the best orthotics are not going to work in bad shoes.”
- ICE, BABY, ICE
Icing, if done correctly, can be a real game-changer, says Doctor of Podiatric Medicine Jenny Ling, and is more effective than oral anti-inflammatories to reduce pain and bring down inflammation.
This is what she tells patients to do:
- Freeze the ice in small paper cups so you have something to hold onto.
- Starting at the heel, massage the painful area with the ice, moving in circular motions.
- Move the ice slowly to different areas, like the arch and then up around the medial malleolus. Be aware of any tenderness, soreness or burning—it indicates inflammation and needs ice massaging.
- When an area feels numb, move to the next area.
- Do the ice massage for 15-to-20 minutes per affected foot, no more.
- Afterwards, even if the pain is gone, rest. ”Don’t go out and run around or play a tennis match because you feel better.”
Resources
Plantar Fasciitis, StatPearls 2024
Ultimate Guide To Plantar Fasciitis
(Pedorthic Association of Canada)
Plantar Fasciitis: Treatment Pearls
(American Academy of Podiatric Sports Medicine)
Exercise and stretching
As noted, plantar fasciitis may be associated with proximal biomechanical factors such as core instability, hip weakness and altered gait mechanics.
Ling points out that in addition to tightness and misalignment, weakness, especially of the core, needs to be addressed.
“The deep abdominal muscles, including the pelvic floor, dictate the stability of your pelvis and your limbs so if there is dysfunction, weakness or tightness, one part will pull on one side and the other side will compensate,” she said. “So an exercise and stretching program is a big part of recovery as well as dealing with the acute inflammation with ice massage.”
Balance and yoga
Balance work and yoga are among the regimes Ling recommends for patients, to treat heel pain (and other foot-related problems) and increase strength and alignment so that it does not return.
Ling believes with targeting icing, the right shoes and orthotics, and the right exercises, the majority of patients can experience a full recovery. She does not recommend night splints to immobilize the foot.
"The premise of these night splints is to put the foot in a dorsiflexed position, to stretch the calf and Achilles overnight. We know that calf tightness rarely occurs in isolation. Usually, the entire posterior chain is involved. A comprehensive stretching and strengthening program would yield better results than using a night splint.”
Platelet-rich plasma injections
In stubborn cases, there are options such as platelet-rich plasma injections and radial shockwave therapy, which Ling prefers over repeated corticosteroid injections due to the risk of plantar fascia rupture and fat pad atrophy with the latter.
“These target the areas of inflammation, like ice, and I tell patients, it can take weeks to see and feel any improvement with these (more advanced) treatments. On the other hand, patients are shocked by how just simple icing, if they do it correctly, can work and work quickly.”